A white paper report in 1966, “Accidental Death and Disability: The Neglected Disease of Modern Society,” documented the lack of emergency medical care and health disparities across the U.S. It found that African Americans had the least access to emergency medical care in the nation, resulting in a public health crisis. Pittsburgh’s largest African American neighborhood, the Hill District, suffered most acutely from this crisis.
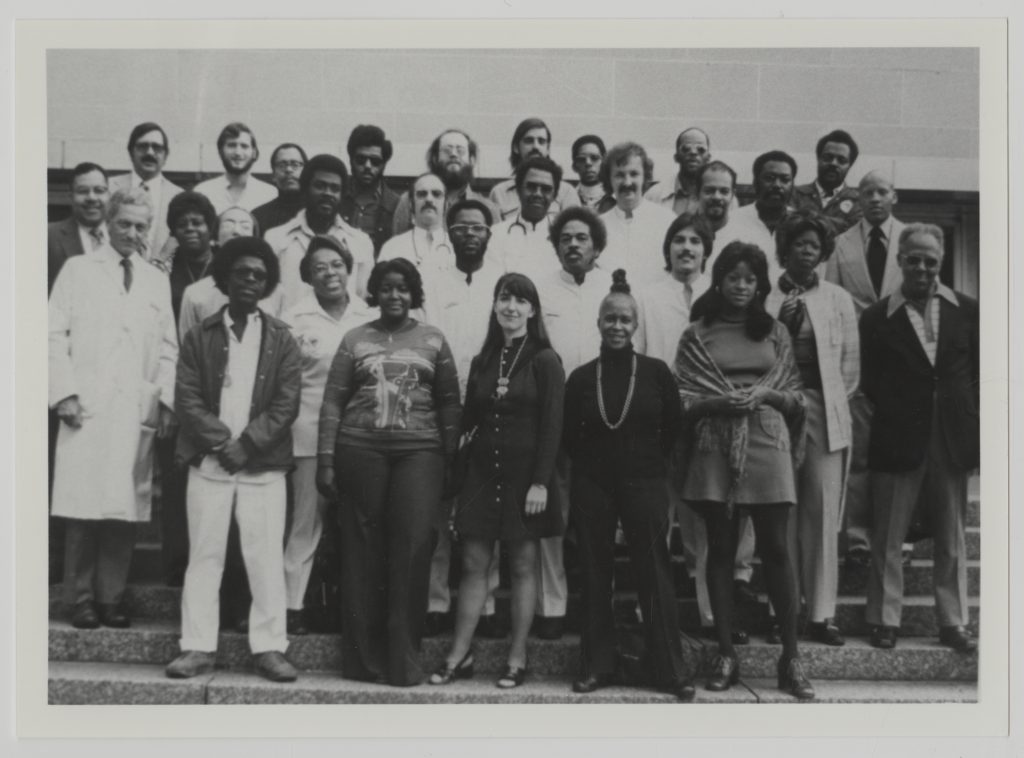
In Pittsburgh the following year, Freedom House Ambulance Service became the nation’s first community-based emergency medical service with trained paramedics. It addressed the urgent need for medical care in the city, especially the Hill District, through a strong collaboration between the Maurice Falk Medical Fund, Freedom House Enterprises (founded by James McCoy, Jr.), and Presbyterian Hospital. Like the community it served, most of its staff were African American.
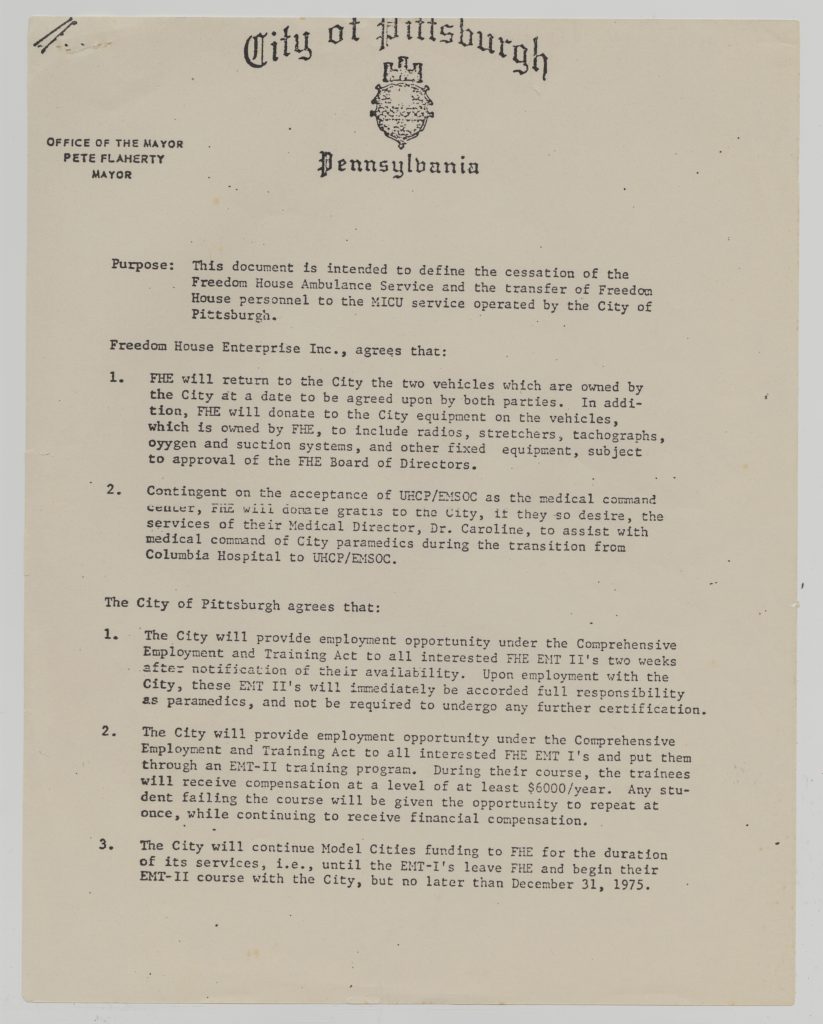
From 1967 to 1975, Freedom House Ambulance Service delivered emergency care to the Hill District, Oakland, and Downtown Pittsburgh, breaking medical ground by training its personnel to previously unheard-of standards. Its paramedics trained under Falk Fund president Phil Hallen and CPR innovator Dr. Peter Safar. The first medical director, Dr. Nancy Caroline, extended the training program and wrote the first textbook for paramedic care, still in use today. As Freedom House medical director, she often rode along with the paramedics and held weekly meetings to review and analyze calls. Her knowledge and training led her to publish emergency medical service manuals and textbooks used by paramedics worldwide.

Freedom House’s five ambulances answered nearly 6,000 calls in the first year, saving more than 200 lives. Its work improved upon the former service by police, funeral homes, fire departments, and private companies not trained or equipped to provide emergency care.
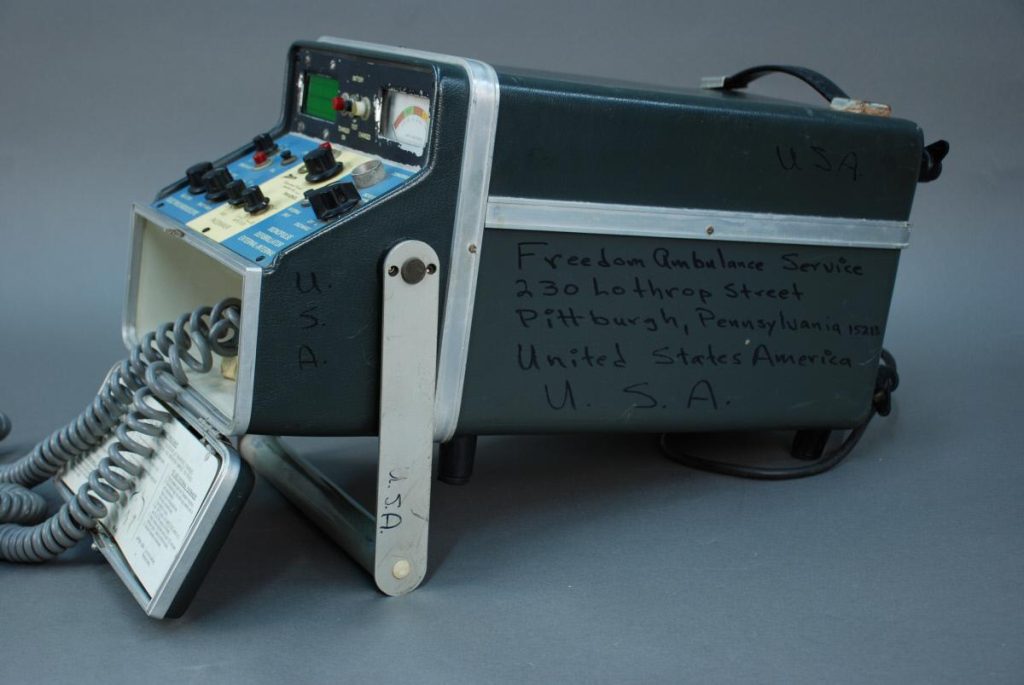
By equipping Freedom House ambulances with medical equipment, the vehicles were transformed into prehospital treatment centers, allowing for innovation in emergency care. Freedom House paramedics became the first to conduct intubation on a patient in the field and to gather data using tools such as a defibrillator to transmit information to the hospital over the radio while in transit. The paramedic training and ambulance design standards pioneered in the Freedom House Ambulance Service laid the foundation for standard emergency treatments.
To this day, the Freedom House legacy lives on. Pittsburgh and the University of Pittsburgh remain centers for the development of innovative training and treatments in emergency services and critical care. In addition, UPMC and UPMC Heath Plan are currently piloting a project, Freedom House 2.0, that is designed to recruit, train, and employ first responders from economically disadvantaged communities, many of which have been significantly impacted by COVID-19. The Freedom House 2.0 program will provide training and support to individuals facing health and economic disparities. The training focuses on traditional emergency medical services and on equipping first responders to address critical, non-emergency psychosocial needs — such as poorly managed chronic medical and behavioral health conditions and a lack of access to resources to address them — that comprise a significant portion of 911 calls. The project echoes Pittsburgh’s original Freedom House initiative in the 1960s and 1970s and aims to transform community health in Western Pennsylvania today.
Visit the Freedom House gallery in the expanded Pittsburgh: A Tradition of Innovation exhibition, made possible with support from UPMC and UPMC Health Plan.